Convert Text to Speech
Topic: Rhesus Factor
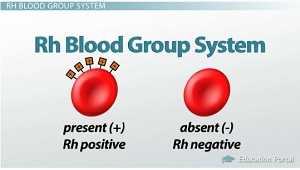
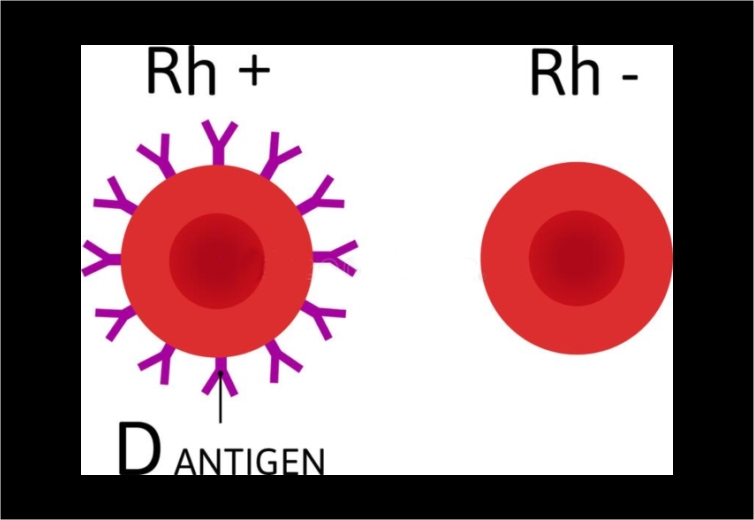
The Rh factor is a protein that can be found on the surface of red blood cells. If your blood cells have this protein it means you are Rh positive but if your blood cells do not have this protein, you are Rh negative.
Why is RH factor important?
Your Rh status does not change a thing but become highly significant during pregnancy, because, problems can occur if you are Rh negative and your fetus is Rh positive.
It can affect the outcome of delivery and determine if a couple with have children. However, treatment can be given to prevent these problems
How do you get a RH factor?
The Rh factor is inherited, meaning it is passed from parent to child through genes. The fetus can inherit the Rh factor from the father or the mother. Most people are Rh positive, meaning they have inherited the Rh factor from either their mother or father. If a fetus does not inherit the Rh factor from either the mother or father, then he or she is Rh negative
When does Rh factor becomes a problem?
When a woman is Rh negative and her fetus is Rh positive, it is called Rh incompatibility.
When the blood of an Rh-positive fetus gets into the bloodstream of an Rh-negative woman, her body will recognize that the Rh-positive blood is not hers. Her body will try to destroy it by making anti-Rh antibodies. These antibodies can cross the placenta and attack the fetus’s blood cells. This can lead to serious health problems, even death, for a fetus or a newborn.
How does this antibodies develop?
The antibodies only develops when there is a blood mixing usually during pregnancy, a woman and her fetus usually do not share blood. But sometimes a small amount of blood from the fetus can mix with the woman’s blood. This can happen during labor and birth. It also can occur with:
-Amniocentesis or Chorionic Villus Sampling (CVS)
-Bleeding during pregnancy
-Attempts to manually turn a fetus so he or she is head-down for birth (move the fetus out of a breech presentation )
-Trauma to the abdomen during pregnancy
*When do the problem becomes a big deal?*
Health problems usually do not occur during an Rh-negative woman’s first pregnancy with an Rh-positive fetus. This is because her body does not have a chance to develop a lot of antibodies. But if treatment is not given during the first pregnancy and the woman later gets pregnant again with an Rh-positive fetus, she can make more antibodies. More antibodies put a future fetus at risk.
Rh antibodies can also develop when a pregnancy is not carried to term such as
• Miscarriage
• Ectopic pregnancy
• Induced abortion
If an Rh-negative woman gets pregnant after one of these events and has not received treatment, a future fetus may be at risk of problems if it is Rh positive.
How can Rh antibodies affect a fetus?
During a pregnancy, Rh antibodies made in a woman’s body can cross the placenta and attack the Rh factor on fetal blood cells. This can cause a serious type of anemia in the fetus in which red blood cells are destroyed faster than the body can replace them.
Red blood cells carry oxygen to all parts of the body. Without enough red blood cells, the fetus will not get enough oxygen. In some cases, a fetus or a newborn can die from anemia.
Rh incompatibility also can cause jaundice in a newborn.
Rh problems is preventable
Problems during pregnancy caused by Rh incompatibility can be prevented. The goal of treatment is to stop an Rh-negative woman from making Rh antibodies in the first place. This is done by finding out if you are Rh negative early in pregnancy (or before pregnancy) and, if needed, giving you a medication to prevent antibodies from forming.
A simple blood test can determine your blood type and Rh status
What is the treatment?
Immunoglobulin (RhIg) is a medication that stops the body from making antibodies if it has not already made them. This can prevent severe fetal anemia in a future pregnancy. RhIg is given as an injection (shot). It is not helpful if your body has already made Rh antibodies.
At 28 weeks of pregnancy—A small number of Rh-negative women may be exposed to Rh-positive blood cells from the fetus in the last few months of pregnancy and may make antibodies against these cells. RhIg given at 28 weeks of pregnancy destroys these Rh-positive cells in the woman’s body. This prevents Rh-positive antibodies from being made.
Within 72 hours after the delivery of an Rh-positive baby—The greatest chance that the blood of an Rh-positive fetus will enter the bloodstream of an Rh-negative woman occurs during delivery. RhIg prevents an Rh-negative woman from making antibodies that could affect a future pregnancy. The treatment is good only for the pregnancy for which it is given. Each pregnancy and delivery of an Rh-positive baby requires a repeat dose of RhIg.
Other times where RhIg is important
• After an ectopic pregnancy, miscarriage, or abortion.
• After amniocentesis, CVS, fetal blood sampling, or fetal surgery
• If you had bleeding during pregnancy
• If you had trauma to the abdomen during pregnancy
• If attempts were made to manually turn a fetus from a breech presentation
Please note
RhIg treatment does not help if an Rh-negative woman has already made antibodies. In this case, the well-being of the fetus will be checked during the pregnancy.
RhIg treatment is not once and for all, it might be necessary for each pregnancy.










Thank you for all your encouraging words and God bless you
Thank God for His unfailing WORD, Hallelujah!!!